For Doctors
Medical science has seen tremendous growth in recent times. Thanks to these developments, millions of people are diagnosed with deadly diseases in time and healed, giving them several more years of life. At LifeGeno, we strive for perfection in diagnosing these diseases.
With the use of the latest technology and state of the art testing equipment, we are able to achieve precision in our diagnostic procedures. Our aim is to be an exemplary laboratory that is recognized for its high efficiency, clinical excellence, professionalism and more importantly, known for being a one stop solution for advanced pathological studies. Over the years in service, we have built a highly advanced testing laboratory which is certified by leading accreditation bodies.
Our strength lies in our implementation of the latest technology. Our labs are equipped with molecular technology including fields such as bioinformatics, pharmocogenomics, companion diagnostics, proteomics and biomarker studies. We also have an integrated research facility, thus helping expand our scope of testing. We welcome specialised consultants including oncologiosts, obstetricians, cardiologists, and physicians who like to do research in any specialized field. Our scientific team would be happy to partner with you for developing & conducting clinical research studies.

Cancer is a genetic disease - that is, cancer is caused by certain changes to genes that control the way our cells function, especially how they grow and divide.
Genes carry the instructions to make proteins, which do much of the work in our cells. Certain gene changes can cause cells to evade normal growth controls and become cancer. For example, some cancer-causing gene changes increase production of a protein that makes cells grow ,mishapen therefore non functional.
Genetic changes that promote cancer can be inherited from our parents if the changes are present in germ cells, which are the reproductive cells of the body (eggs and sperm). Cancer-causing genetic changes can also be acquired during one’s lifetime, as the result of errors that occur as cells divide or from exposure to carcinogenic substances that damage DNA, such as certain chemicals in tobacco smoke, and radiation, such as ultraviolet rays from the sun. Genetic changes that occur after conception are called somatic (or acquired) changes. One nucleotide may be replaced by another, or it may be missing entirely, or deletions, duplications.
Hereditary Cancer Syndromes
Inherited genetic mutations play a major role in about 5 to 10 percent of all cancers. Researchers have associated mutations in specific genes with more than 50 hereditary cancer syndromes, which are disorders that may predispose individuals to developing certain cancers. Genetic tests for hereditary cancer syndromes can tell whether a person from a family that shows signs of such a syndrome has one of these mutations. These tests can also show whether family members without obvious disease have inherited the same mutation as a family member who carries a cancer-associated mutation.
Genetic testing for cancer risk be considered when someone has a personal or family history that suggests an inherited cancer risk condition, as long as the test results can be adequately interpreted (that is, they can clearly tell whether a specific genetic change is present or absent) and when the results provide information that will help guide a person’s future medical care.
Here are examples of genes that can play a role in hereditary cancer syndrome:
TP53
which produces a protein that suppresses the growth of tumors. In addition, germline mutations in this gene can cause Li-Fraumeni syndrome, a rare, inherited disorder that leads to a higher risk of developing certain cancers.
BRCA1 and BRCA2
are associated with hereditary breast and ovarian cancer syndrome, which is a disorder marked by an increased lifetime risk of breast and ovarian cancers in women.PTEN
Mutations in this gene are associated with Cowden syndrome, an inherited disorder that increases the risk of breast, thyroid, endometrial, and other types of cancer.
Genetic Tests for Hereditary Cancer Syndromes

Genetic tests for mutations that cause hereditary cancer syndromes are usually requested by a person’s doctor or other health care provider. Genetic counseling can help people consider the risks, benefits, and limitations of genetic testing in their particular situations.
A genetic counselor, doctor, or other health care professional trained in genetics can help an individual or family understand their test results and explain the possible implications of test results for other family members.
Identifying Genetic Changes in Cancer
Lab tests called DNA sequencing tests can “read” DNA. By comparing the sequence of DNA in cancer cells with that in normal cells, such as blood or saliva, scientists can identify genetic changes in cancer cells that may be driving the growth of an individual’s cancer. Indeed, in some cases, the genetic testing of tumors has shown that a patient’s cancer could be associated with a hereditary cancer syndrome that the family was not aware of.
Genetic diseases are not as rare as once believed. In fact, genetic disease is a major cause of illness and death. Approximately 2% to 3% of all pregnancies result in a neonate with a serious genetic disease or a birth defect that can cause disabilities, mental retardation, and in some cases early death. Genetic factors are present from conception, and their expression may vary throughout development, whereas environmental influences are changing constantly.
Genetically determined disorders often are subdivided into 3 major groups: single gene, chromosome, and multifactorial (polygenic) diseases. Somatic cell genetic defects play a role in human cancer and constitute a fourth group. Single-gene disorders This type is caused by changes or mutations that occur in the DNA sequence of one gene.
Considering that the human genome consists of approximately 30,000 genes, the number of diseases classified as monogenic is expected to increase. Compared to general population, the risk of occurrence of genetic diseases in affected families is very high depending on the pattern of inheritance. However, previous occurrence of the disease in the family is not necessary. The defect may arise de novo for the first time in any individual or there may be silent carriers in the family who give birth to an affected child without a positive family history (autosomal recessive disorder). The four most common patterns of mendelian inheritance are based primarily on two factors: on which type of chromosome (autosome or sex chromosome) the gene locus is found and whether the phenotype is expressed only when both chromosomes of a pair carry the abnormal allele (recessive) or whether the phenotype can be expressed when just one chromosome carries the mutant allele (dominant).
Single-gene disorders are inherited in recognizable patterns: autosomal dominant, autosomal recessive, and X-linked. . Genetic technology is advancing rapidly, bringing new, safer and more sensitive ways to diagnose genetic conditions pre- and postnatally. These advances will bring about profound changes in the way we deliver obstetric services to women and their families.Diagnosing a genetic disorder not only allows for disease-specific management options but also has implications for the affected individual’s entire family. Hence, a working understanding of the underlying concepts of genetic disease is important for all practicing clinicians. Although it is impossible to know all aspects of clinical and molecular genetics, basic knowledge of certain topics is a must for all practicing obstetricians.
Clinical genetics is one of the most rapidly advancing fields in medicine. Spectacular progress has been achieved in this century with unravelling of the entire draft sequence of the human genome. A major contribution of these advances has been in diagnosis, management and prenatal diagnosis of genetic disorders as treatment in most cases is difficult or impossible and where available beyond the means of most families. Genetic technology is advancing rapidly, bringing new, safer and more sensitive ways to diagnose genetic conditions pre- and postnatally.
These advances will bring about profound changes in the way we deliver obstetric services to women and their families. Diagnosing a genetic disorder not only allows for disease-specific management options but also has implications for the affected individual's entire family. Hence, a working understanding of the underlying concepts of genetic disease is important for all practicing clinicians. Although it is impossible to know all aspects of clinical and molecular genetics, basic knowledge of certain topics is a must for all practicing obstetrician/gynecologists
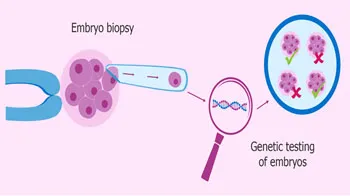
Preimplantation genetic testing (PGT) is a technique in which one or more cells are taken from an egg or embryo (fertilized egg) for testing to provide information about the genetic make-up of the rest of the cells in that embryo. Specifically, this would include patients with a history of single-gene disorders (such as cystic fibrosis or sickle cell anemia) and patients with a history of sex-linked disorders (such as Duchenne muscular dystrophy and Fragile X syndrome). In addition, even families in search of a bone marrow donor may be able to use PGT to bring a child into the world that can provide matching stem cells for an affected sibling.
Types of PGT testing-
PGT A (Aneuploidy)
Checks for extra or missing chromosomes.
PGT M (Monogenic)
Checks for single-gene mutations to reduce the risk of couples with known inherited condition caused by mutations in a single gene such as Huntington disease.
PGT SR (Structural Rearrangement)
It is used to detect unbalanced chromosome rearrangements
Cells from the embryo can be tested for a gene that may produce a specific disease. This will show if an embryo is normal (no disease) or affected (has the disease). It will also show if the embryo is carrying the disease but unaffected by it. An unaffected carrier is someone who can pass the disease to his or her children but does not personally have any signs of the disease A karyotype is another kind of genetic test that can check the chromosomes. It is done during pregnancy, either by a chorionic villus sampling or amniocentesis. This test shows if the fetus has more or fewer chromosomes than the usual 46. Having too many or too few chromosomes can cause disorders such as Down syndrome (Trisomy 21) or Trisomy 13.
DETERMINATION OF SEX OF THE FETUS OR EMBRYO IS NOT CARRIED OUT HERE!

Genetic testing looks for changes, sometimes called mutations or variants, in your DNA. Genetic testing is useful in many areas of medicine and can change the medical care you or your family member receives.Because we share DNA with our family members, if you are found to have a genetic change, your family members may have the same change. Genetic Counselling before and after genetic testing can help make sure that you are the right person in your family to get a genetic test, you’re getting the right genetic test, and that you understand your results.
As the medicine and genetics go hand in hand it is important for the physician of the treating doctor to exactly know or to rule out and disorder, condition especially in certain types of cancer which has been inherited through genes or due to any alterations in the genetic makeup. Genetic testing makes it simplified to rule out conditions that are tedious or not possible by any other methodologies.Early discovery will also aid their management.
- To learn whether you have a genetic condition that runs in your family before you have symptoms
- To learn about the chance a current or future pregnancy will have a genetic condition
- To diagnose a genetic condition if you or your child has symptoms
- To understand and guide your cancer prevention or treatment plan
There are many different kinds of genetic tests. There is no single genetic test that can detect all genetic conditions. The approach to genetic testing is individualized based on your medical and family history and what condition you’re being tested for.
- Single gene testing -
Single gene tests look for changes in only one gene .Some examples of this are Duchene muscular dystrophy or sickle cell disease. Single gene testing is also used when there is a known genetic mutation in a family. - Panel testing-
A panel genetic test looks for changes in many genes in one test. Genetic testing panels are usually grouped in categories based on different kinds of medical concerns. Some examples of genetic panel tests are low muscle tone, short stature, or epilepsy. Panel genetic tests can also be grouped into genes that are all associated with higher risk of developing certain kinds of cancer, like breast or colorectal (colon) cancer. - Large-scale genetic or genomic
testing-
There are two different kinds of large-scale genetic tests.- Exome sequencing looks at all the genes in the DNA (whole exome) or just the genes that are related to medical conditions (clinical exome).
- Genome sequencing is the largest genetic test and looks at all of a person’s DNA, not just the genes
Large scale tests are prescribed to those patients with complex medical histories. Large-scale genomic testing is also used in research to learn more about the genetic causes of conditions.
If you would like to customize a panel with few frequently prescribed tests, please feel free to get in touch with us. We would be happy to work with you on the same.
